What is sciatica?
Sciatica is pain caused by irritation or compression of the sciatic nerve, the longest and thickest nerve in the body. The sciatic nerve starts in the lower spine and runs through the buttock and down the back of the leg to the foot.
Sciatica is not a diagnosis itself, but a set of symptoms caused by an underlying spinal or nerve condition.
Where is sciatic pain felt?
Symptoms can occur in:
Lower back
Buttock
Back or side of the thigh
Calf
Foot and toes
Pain usually affects one side of the body.
Common symptoms
Sharp, burning, or electric-shock–like pain
Pain that radiates down the leg
Pins and needles (tingling)
Numbness
Muscle weakness in the leg or foot
Pain worsened by coughing, sneezing, bending, or sitting
⚠️ Red flag symptoms (urgent medical review required):
Loss of bladder or bowel control
Progressive leg weakness
Severe numbness in the groin or saddle area
Types of sciatica
True sciatica
Direct compression or irritation of the sciatic nerve
Sciatica-like pain
Symptoms mimic sciatica but originate from nearby nerves or structures
In clinical practice, both are commonly referred to as “sciatica.”
Common causes
Slipped (herniated) disc
Degenerative disc disease
Spinal or foraminal stenosis
Spondylolisthesis
Osteoarthritis
Trauma or injury
Pregnancy
Tumours or cysts (rare)
Cauda equina or conus medullaris syndrome (emergency)
Risk factors
Poor posture and lifting technique
Prolonged sitting or inactivity
Weak core muscles
Excess body weight
Heavy manual work
Smoking
Diabetes
Age-related spinal changes
How is sciatica diagnosed?
Clinical assessment (history + physical examination)
Gait observation
Straight leg raise test
Neurological examination (strength, reflexes, sensation)
MRI scan is indicated if:
Symptoms persist
Severe pain or weakness is present
Multiple nerve roots are suspected
Red flags are identified
Treatment options
Self-management (mild cases)
Ice (first 48–72 hours)
Heat thereafter
NSAIDs (if appropriate)
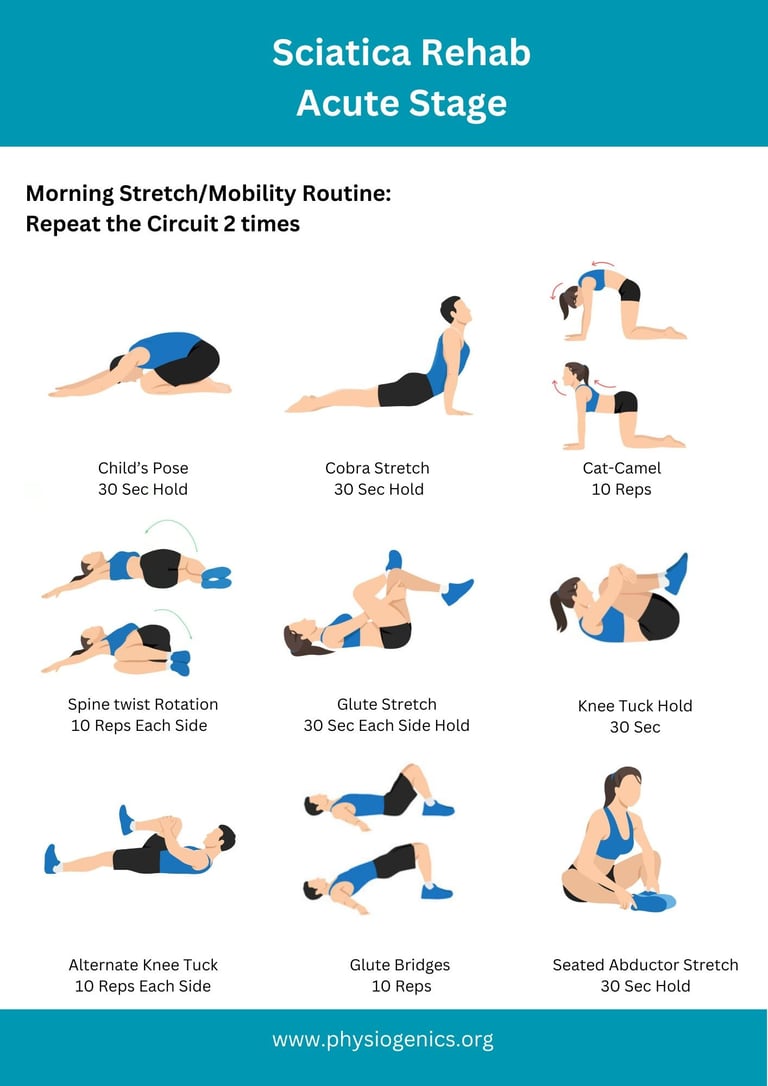
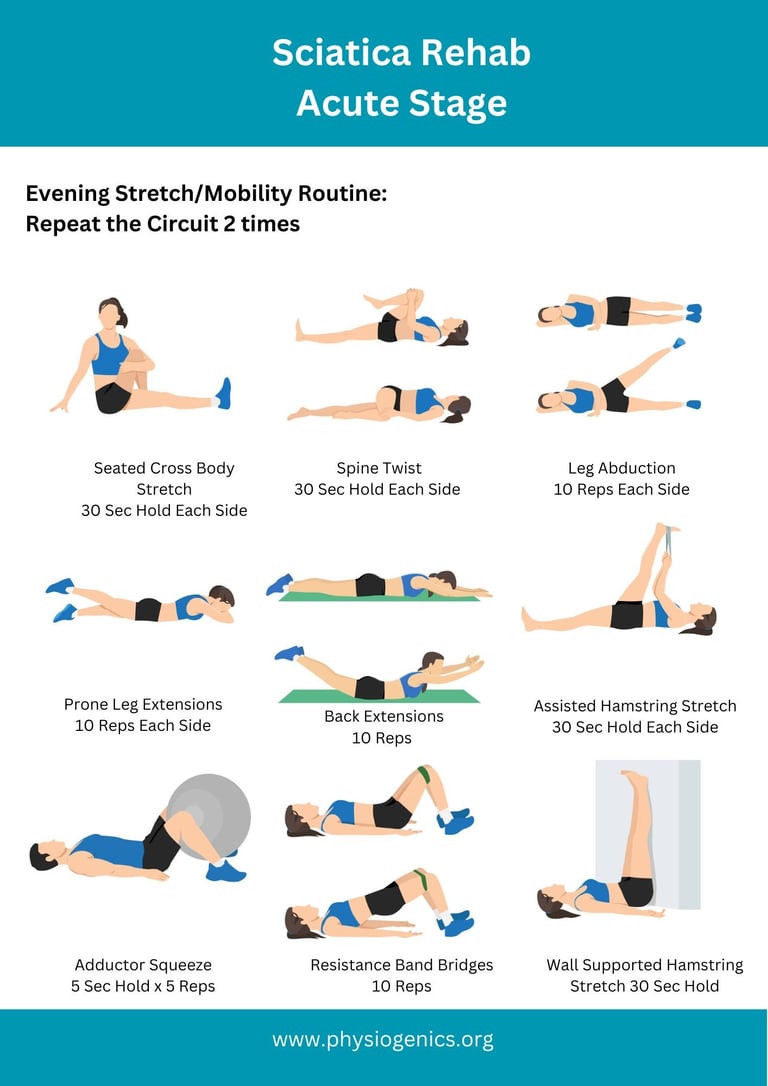
Gentle mobility and stretching
Staying active (avoid prolonged bed rest)
Conservative treatment
Physiotherapy (exercise-based rehab)
Prescription pain relief or nerve medications
Spinal injections (short-term relief)
Acupuncture, chiropractic care, massage (adjuncts)
Surgery (only if needed)
Considered when:
Severe or worsening neurological symptoms
Persistent pain beyond 6–8 weeks
Failure of conservative treatment
Common procedures:
Discectomy
Laminectomy
Prognosis
Most people recover fully
Some may develop chronic pain
Rarely, permanent nerve damage can occur if untreated
Can sciatica be prevented?
Risk can be reduced by:
Maintaining good posture
Regular exercise and core strengthening
Healthy body weight
Safe lifting techniques
Staying physically active
Physiotherapy Exercises for Acute Sciatica: 3-4 weeks