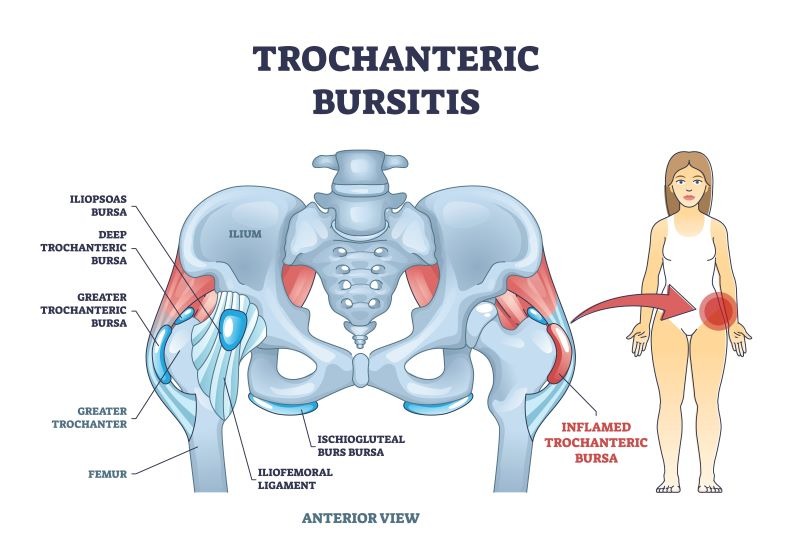
Trochanteric bursitis refers to inflammation of the bursa located over the greater trochanter on the outer aspect of the hip. The bursa acts as a fluid-filled cushion between bone and surrounding soft tissues, reducing friction—similar to protective “bubble wrap” for the joint.
The most common symptom is pain on the outside of the hip, which may:
Radiate into the outer thigh or buttock.
Worsen when lying on the affected side.
Increase after standing from prolonged sitting.
Increase with hip movement, especially stair climbing or long-distance walking.
Trochanteric bursitis can develop from anything that irritates the bursa, including:
Repetitive stress: frequent stair climbing, running, cycling, heavy lifting, or prolonged standing.
Direct trauma: falls, bumps, or lying on one side for long periods.
Biomechanical/postural issues: scoliosis, leg-length discrepancy, hip bone spurs, altered pelvic/lumbar mechanics.
Overuse or tendon friction from gluteal tendinopathy.
Higher risk occurs in:
Athletes and people doing frequent manual work.
Over-weight/obese individual as it leads to swaying of hip side to side during walking due to weakness in hip muscles (glutes)
Individuals with previous hip surgery.
Those with underlying conditions such as:
Osteoarthritis / inflammatory arthritis (gout, psoriatic arthritis)
Psoriasis
Diabetes
Thyroid disorders
Trochanteric bursitis is primarily diagnosed through a clinical examination. A clinician will assess:
Symptom history and aggravating factors
Local tenderness over the greater trochanter
Hip range of motion and functional testing
Management
Most cases improve with conservative treatment:
Rest / activity modification: avoiding positions or tasks that overload the hip.
Analgesia: short-term use of ibuprofen, naproxen, or paracetamol (seek guidance before using for >10 days).
Off-loading aids: temporary use of a cane or crutches if walking is painful.
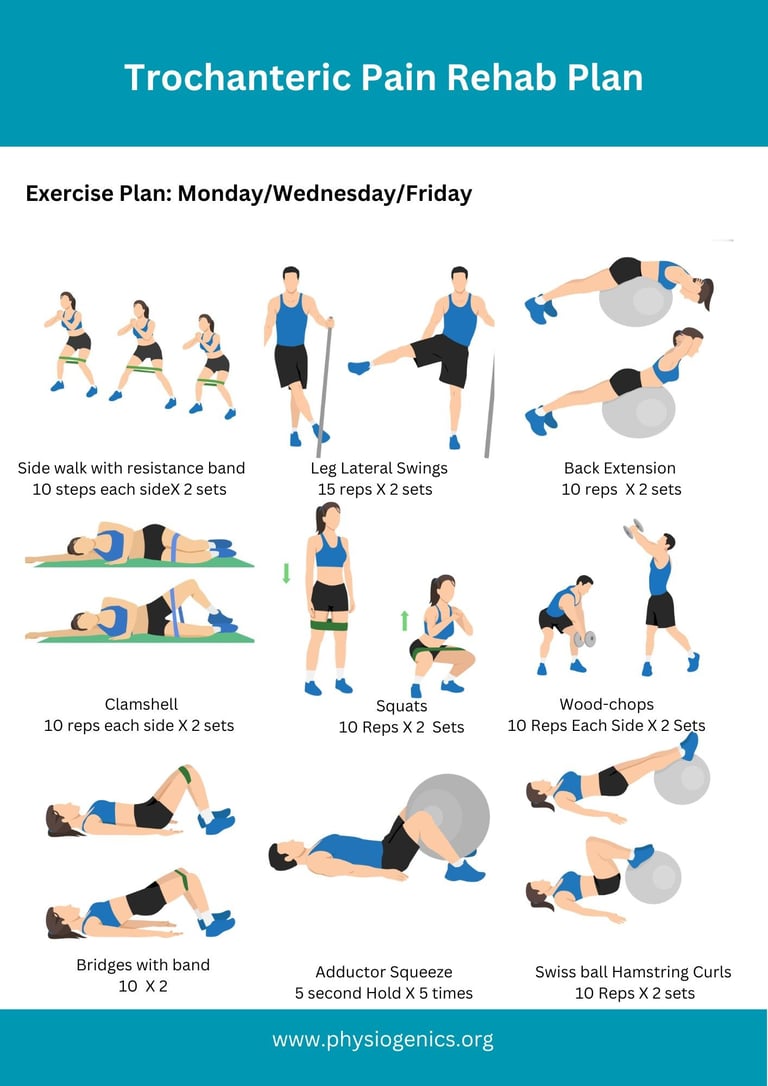
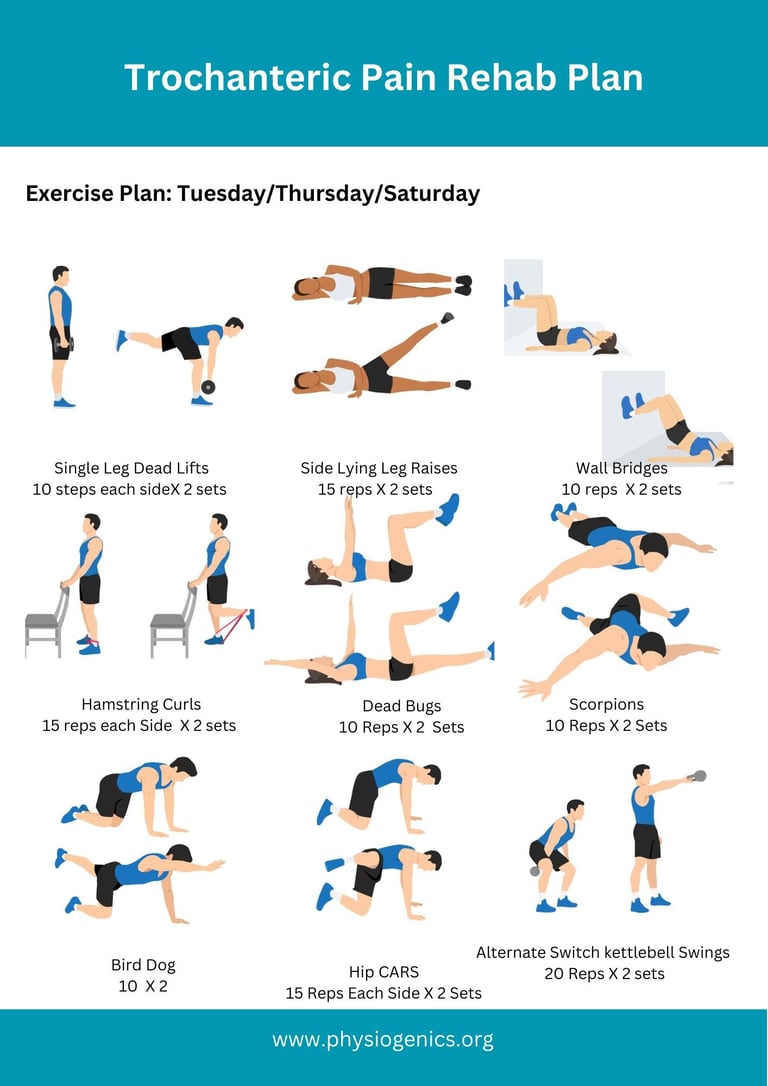
Physiotherapy:
Gluteal strengthening
ITB stretching
Hip mobility work
Gait/postural correction
If conservative management did not have positive outcomes then:
Corticosteroid injection: reduces inflammation and provides short-term pain relief.
Surgery: extremely rare; considered only after >6 months of failed conservative management.
Consult a healthcare provider if hip pain:
Persists beyond 2–3 weeks
Is worsening
Interferes significantly with walking, sleep, or daily activities