What is frozen shoulder?
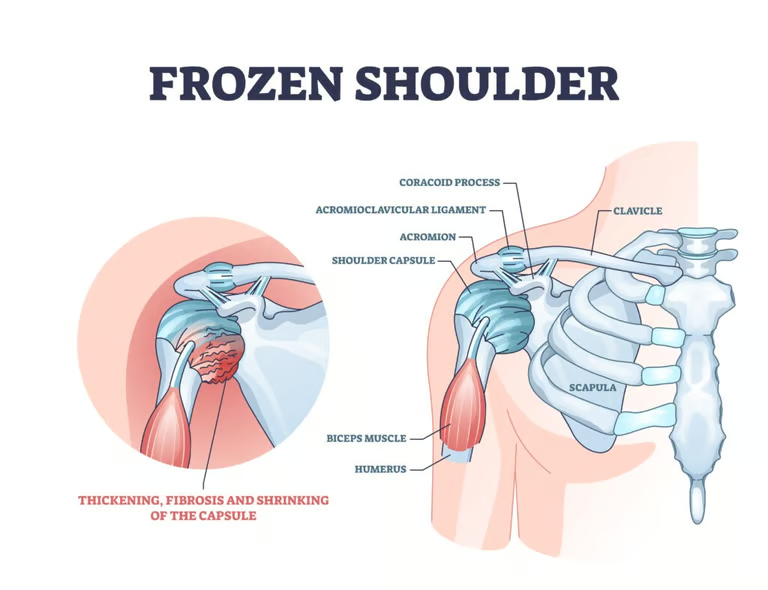
Frozen shoulder happens when the shoulder joint capsule (the strong connective tissue that surrounds and stabilises the shoulder) becomes inflamed and stiff. Over time, scar tissue (adhesions) forms and the lubricating joint fluid reduces, severely limiting movement.
The shoulder is called “frozen” because pain leads to reduced use, which then causes further stiffness and loss of movement.
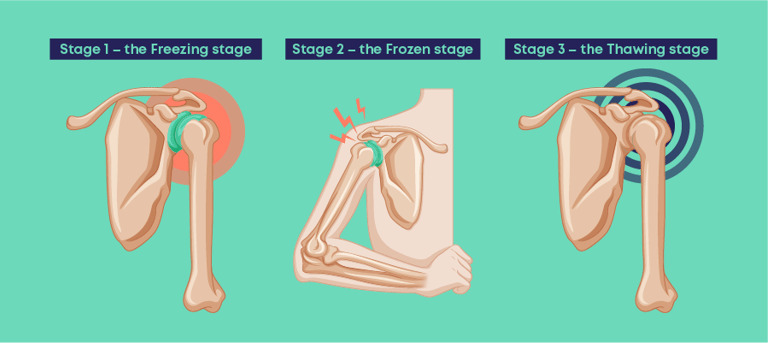
Stages of frozen shoulder
Freezing: Increasing pain, stiffness, worse at night, movement gradually reduces- 6 weeks – 9 months
Frozen: Pain may reduce, but stiffness is severe and daily tasks are difficult- 2- 6 months
Thawing: Pain settles, movement gradually improves- 6 months – 2 years
Causes
The exact cause is unknown, but inflammation leads to:
Thickened and tight joint capsule
Scar tissue (adhesions)
Reduced joint lubrication
This combination restricts shoulder movement in all directions.
Risk factors
You’re more likely to develop frozen shoulder if you have:
Age: 40–60 years
Sex: More common in females
Shoulder immobilisation: After injury or surgery (e.g. sling use)
Diabetes: 10–20% of people with diabetes are affected
Other conditions: Stroke, thyroid disorders, Parkinson’s disease, heart disease
Symptoms
Shoulder pain (often worse at night)
Progressive stiffness
Difficulty lifting the arm, dressing, grooming, or reaching overhead
Loss of both active and passive range of motion
Diagnosis
Frozen shoulder is diagnosed through:
Clinical history and symptom pattern
Physical examination showing reduced active and passive movement
X-rays to rule out arthritis
MRI or ultrasound only if another condition (e.g. rotator cuff tear) is suspected
Treatment
Treatment focuses on pain control first, then restoring movement.
Conservative treatment (most common)
Pain relief (NSAIDs, paracetamol)
Corticosteroid injection into the shoulder joint- Steroid Injections are considered early as the condition might get chronic.
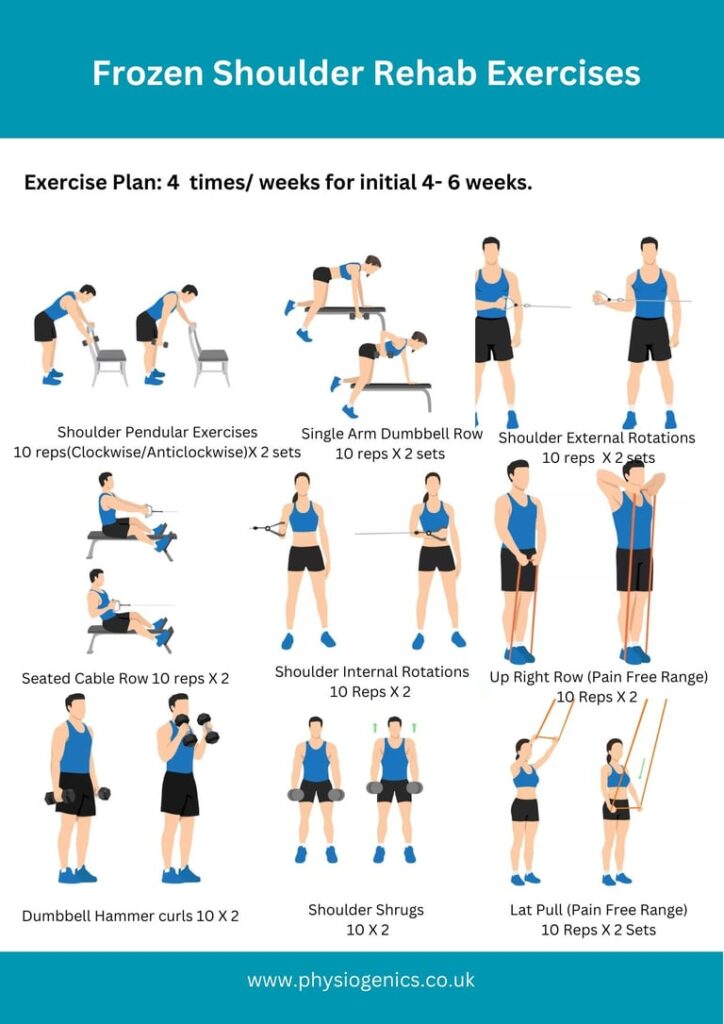
Physical therapy (stretching & mobility exercises)
Home exercise program
Heat/ice
TENS for pain relief
Surgical options (if symptoms persist >12 months)
Manipulation under anaesthesia
Arthroscopic capsular release
(often combined for better results)
Prognosis
Most people recover without surgery
Improvement usually occurs within 12 months
Full or near-full recovery may take up to 2 years
Even untreated cases gradually improve, though more slowly
Understand Your Shoulder Movements: What movements are restricted and painful.
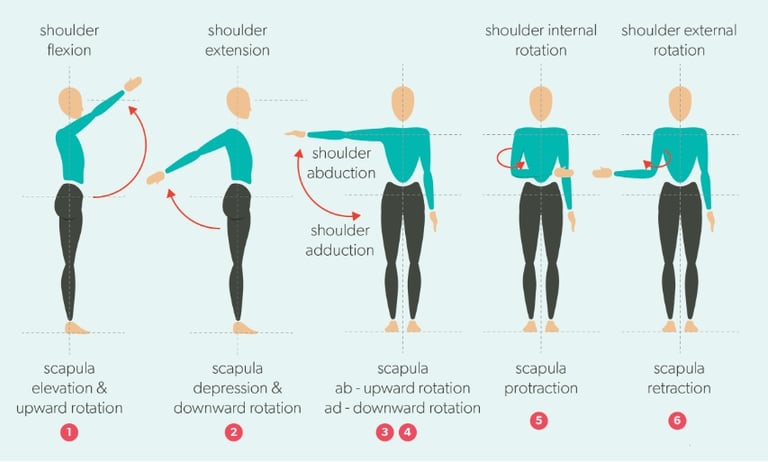
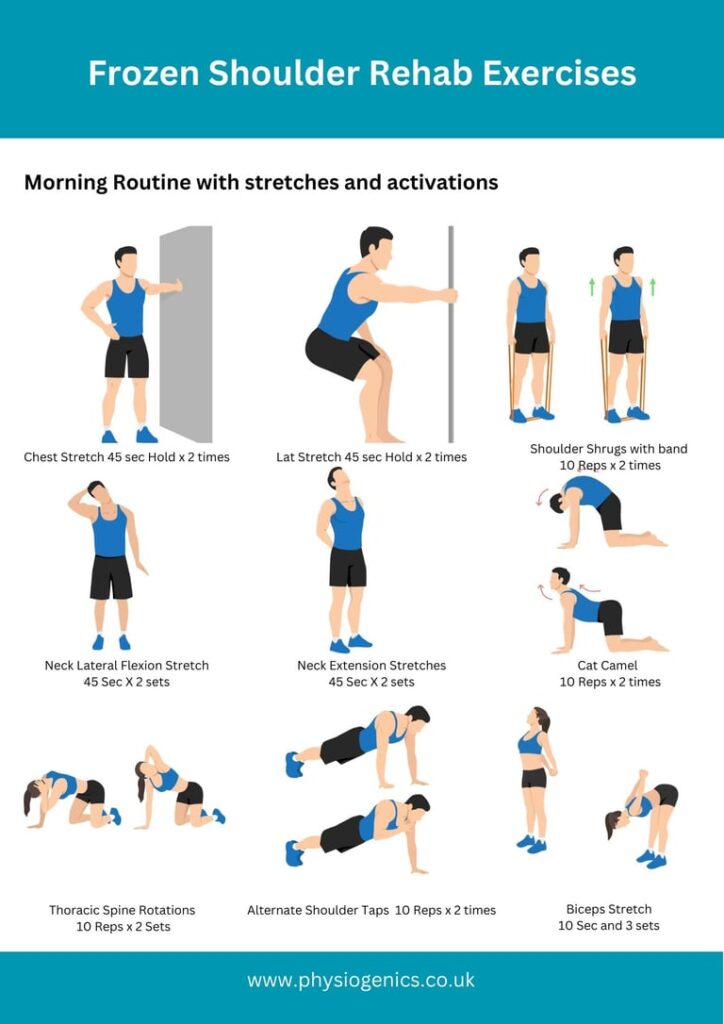
Physiotherapy Rehab Exercises