What Is a Stroke?
A stroke is a medical emergency that happens when blood flow to part of the brain is blocked or when a blood vessel in the brain ruptures. Without oxygen-rich blood, brain cells begin to die within minutes, which can cause permanent brain damage or death.
Strokes are also called cerebrovascular accidents (CVAs) or brain attacks.
Brain cells die quickly without oxygen
Damage can become permanent
Fast treatment can save life and brain function
Every second matters
Common Stroke Symptoms
Symptoms depend on which part of the brain is affected, but common signs include:
Weakness or paralysis on one side of the body or face
Trouble speaking or understanding speech (aphasia, slurred speech)
Vision problems (blurred or double vision)
Sudden confusion or memory loss
Severe, sudden headache
Dizziness, loss of balance, or coordination problems
Nausea, vomiting, seizures, or loss of consciousness
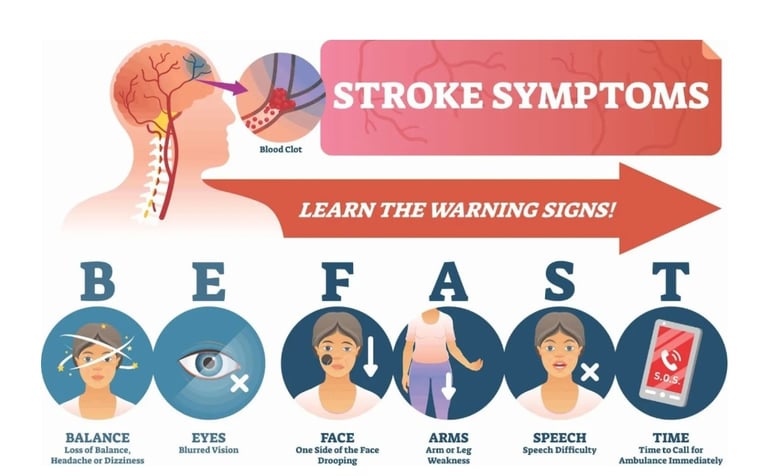
Warning Signs: BE FAST
Use BE FAST to recognize a stroke quickly:
Balance – sudden loss of balance
Eyes – sudden vision problems
Face – face drooping
Arms – arm weakness or drifting
Speech – slurred or difficult speech
Time – call emergency services immediately
❌ DON’Ts
1. ❌ Do NOT Pull the Affected Arm
Never lift or turn the patient by the affected arm
Avoid pulling during transfers
➡ Can cause shoulder subluxation and pain
2. ❌ Avoid Forceful Stretching
No jerky or fast movements
No pushing into pain
➡ Can increase spasticity and cause injury
3. ❌ Do NOT Ignore the Affected Side
Don’t let the patient use only the strong side
Encourage looking at, touching, and moving the affected side
4. ❌ Avoid Prolonged Poor Positioning
No dangling arm unsupported
No prolonged wrist/finger flexion
No ankle left in plantarflexion (foot drop risk)
5. ❌ No Resistance Exercises Early On
Avoid weights or strong resistance
Especially if muscle tone is flaccid or just emerging
6. ❌ Don’t Over-Fatigue
Stop if:
Increased weakness
Dizziness
Excessive spasticity
Pain
Fatigue slows recovery.
Warning Signs – Stop and Seek Medical Advice
Sudden increase in weakness
Severe shoulder pain
New confusion or headache
Chest pain or breathlessness
Swelling or redness in leg (possible DVT)
Key Principles to Remember
Early, gentle, repetitive movement
Quality over quantity
Use the affected side safely
Consistency every day
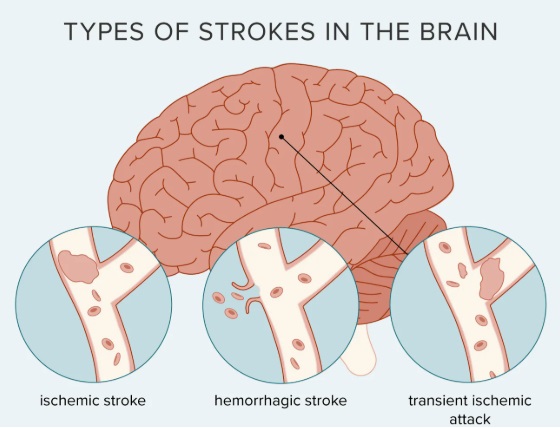
Types of Stroke
1. Ischemic Stroke (Most Common)
Caused by a blood clot blocking a vessel supplying the brain.
Common causes:
Atherosclerosis (hardened arteries)
Atrial fibrillation
Heart defects
Clotting disorders
2. Haemorrhagic Stroke
Caused by bleeding in the brain due to a ruptured blood vessel.
Common causes:
High blood pressure
Brain aneurysm
Brain tumors
Blood vessel diseases (e.g., Moyamoya disease)
3. Transient Ischemic Attack (TIA)
“Mini-stroke”
Symptoms are temporary
Major warning sign of a future stroke
Requires emergency care
Risk Factors
Higher risk if you:
Are over 65
Smoke or vape
Use drugs or excessive alcohol
Medical conditions increasing risk:
High blood pressure
High cholesterol
Diabetes
Migraines
COVID-19
Heart conditions
Diagnosis
Doctors diagnose strokes using:
Neurological exams
CT scan or MRI
Blood tests
EKG / EEG
Treatment
Treatment depends on stroke type and severity:
Ischemic Stroke
Clot-busting drugs (thrombolytics)
Mechanical thrombectomy
Blood pressure control
Haemorrhagic Stroke
Medications to stop bleeding
Blood pressure management
Surgery to reduce brain pressure
Stroke Rehabilitation
Recovery often requires:
Physical therapy
Occupational therapy
Speech therapy
Cognitive rehabilitation
Rehab helps regain skills or adapt to changes.
Recovery & Prognosis
Recovery varies from person to person
Many recover over months
Faster treatment = better outcomes
Ischemic strokes usually have better survival than haemorrhagic strokes
Stroke Prevention
You can lower your risk by:
Eating healthy
Exercising regularly
Controlling blood pressure, cholesterol, and diabetes
Quitting smoking
Seeing your doctor regularly
When to Go to the ER
Call emergency services immediately if:
You notice stroke symptoms
Symptoms return after a stroke
You have signs of complications (chest pain, breathing trouble, seizures)
Questions to Ask Your Doctor
What type of stroke did I have?
Will I have long-term effects?
What rehab do I need?
What signs of another stroke should I watch for?
2. Passive & Assisted Range of Motion (ROM)
Performed slowly, pain-free, 1–2 times/day.
Upper Limb
Shoulder flexion, abduction, external rotation
Elbow flexion/extension
Forearm pronation/supination
Wrist and finger extension (important to prevent flexor tightness)
Lower Limb
Hip flexion/extension, abduction
Knee flexion/extension
Ankle dorsiflexion/plantarflexion
👉 Move all joints, not just the paralyzed ones.
3. Early Active or Active-Assisted Exercises (as soon as possible)
Even minimal effort counts.
Shoulder shrugs
Scapular protraction/retraction
Assisted reaching
Assisted hip and knee bending
Ankle pumps
Use:
The unaffected hand to assist the affected hand
Therapist or caregiver assistance
4. Bed Mobility & Postural Control
Rolling side to side
Bridging (lifting hips)
Supported sitting at edge of bed
Weight shifting in sitting
These are functional exercises that speed recovery.
5. Sensory Stimulation
Light touch, tapping, brushing
Joint compression (gentle)
Different textures (cloth, sponge)
Helps brain re-mapping (neuroplasticity).
6. Breathing Exercises
Deep breathing
Incentive spirometry (if available)
Assisted coughing
Prevents chest infections.
7. Short, Frequent Sessions
10–20 minutes
2–4 times/day
Rest between exercises
Fatigue is common after stroke.
Goals of the Initial Phase (first days–weeks)
Prevent joint stiffness, contractures, and shoulder subluxation
Maintain range of motion
Promote early activation of the affected side
Improve postural control and bed mobility
Prevent complications (pressure sores, chest infection, DVT)
✅ DO’s
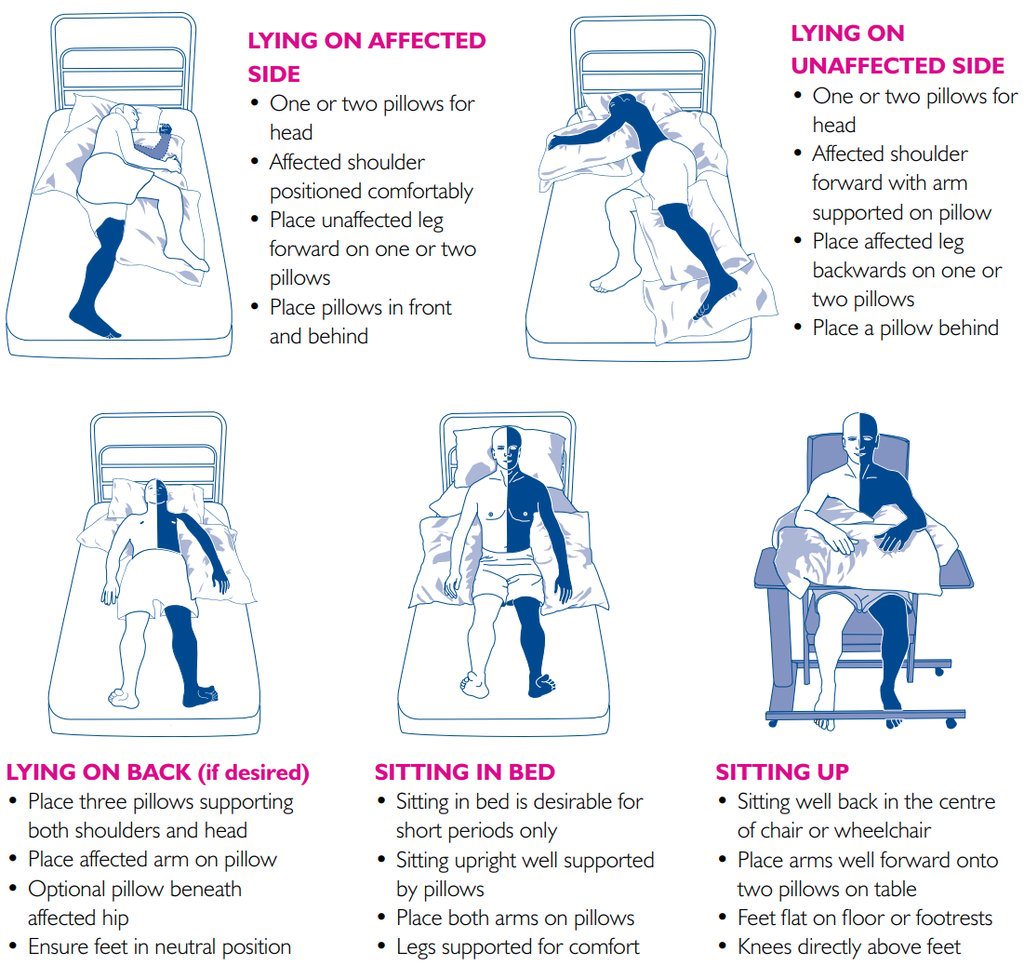
1. Positioning (VERY IMPORTANT)
Proper positioning should be done 24 hours/day.
In bed:
Keep the affected shoulder supported (pillow under arm, shoulder slightly forward)
Affected arm:
Shoulder slightly abducted and externally rotated
Elbow extended
Wrist neutral
Fingers gently extended
Affected leg:
Hip neutral/slight flexion
Knee slightly flexed
Ankle supported in neutral (foot board or pillow)
Side-lying on affected side (if tolerated):
Encourages weight bearing and sensory input
Affected shoulder positioned forward (not underneath the body)
2. Passive & Assisted Range of Motion (ROM)
Performed slowly, pain-free, 1–2 times/day.
Upper Limb
Shoulder flexion, abduction, external rotation
Elbow flexion/extension
Forearm pronation/supination
Wrist and finger extension (important to prevent flexor tightness)
Lower Limb
Hip flexion/extension, abduction
Knee flexion/extension
Ankle dorsiflexion/plantarflexion
👉 Move all joints, not just the paralyzed ones.
3. Early Active or Active-Assisted Exercises (as soon as possible)
Even minimal effort counts.
Shoulder shrugs
Scapular protraction/retraction
Assisted reaching
Assisted hip and knee bending
Ankle pumps
Use:
The unaffected hand to assist the affected hand
Therapist or caregiver assistance
4. Bed Mobility & Postural Control
Rolling side to side
Bridging (lifting hips)
Supported sitting at edge of bed
Weight shifting in sitting
These are functional exercises that speed recovery.
5. Sensory Stimulation
Light touch, tapping, brushing
Joint compression (gentle)
Different textures (cloth, sponge)
Helps brain re-mapping (neuroplasticity).
6. Breathing Exercises
Deep breathing
Incentive spirometry (if available)
Assisted coughing
Prevents chest infections.
7. Short, Frequent Sessions
10–20 minutes
2–4 times/day
Rest between exercises
Fatigue is common after stroke.
❌ DON’Ts
1. ❌ Do NOT Pull the Affected Arm
Never lift or turn the patient by the affected arm
Avoid pulling during transfers
➡ Can cause shoulder subluxation and pain
2. ❌ Avoid Forceful Stretching
No jerky or fast movements
No pushing into pain
➡ Can increase spasticity and cause injury
3. ❌ Do NOT Ignore the Affected Side
Don’t let the patient use only the strong side
Encourage looking at, touching, and moving the affected side
4. ❌ Avoid Prolonged Poor Positioning
No dangling arm unsupported
No prolonged wrist/finger flexion
No ankle left in plantarflexion (foot drop risk)
5. ❌ No Resistance Exercises Early On
Avoid weights or strong resistance
Especially if muscle tone is flaccid or just emerging
6. ❌ Don’t Over-Fatigue
Stop if:
Increased weakness
Dizziness
Excessive spasticity
Pain
Fatigue slows recovery.
Warning Signs – Stop and Seek Medical Advice
Sudden increase in weakness
Severe shoulder pain
New confusion or headache
Chest pain or breathlessness
Swelling or redness in leg (possible DVT)
Key Principles to Remember
Early, gentle, repetitive movement
Quality over quantity
Use the affected side safely
Consistency every day